Analysing the economic burden of COVID-19 patient hospitalization and testing: a comparison between Austria and Finland
Flammer Julian, Kollmann Birgit, Kristof Verena, Pratl Bernadette, Salobir Helene, Järvinen Sari
The novel SARS-CoV-2 virus spread around the world in early 2020, what is now known as the “Covid-19” pandemic. Due to this governments around the world rushed to implement various policy actions in an attempt to protect health while minimizing economic damage. In Europe there was no cooperation working across the different states and this resulted in different considerably between countries (Desson et al., 2020). In many countries the effects of the pandemic results in restrictions as lockdowns, mobility restrictions, stay-at-home orders, financial rescue packages, interstate tensions, state border closings, digital surveillance and the concentration of infections in cities. In Finland, the state banned gatherings of more than ten people, closed the borders of the state, closed schools, universities, museums, restaurants and libraries and even the borders of the Uusimaa province for a limited period of time in order to prevent the spread of COVID-19 (Moisio, 2020).
Furthermore, the pandemic had a big impact on the health care system due to the huge amount of hospital resources (ICU beds, nursing staff, invasive ventilators) which were needed to manage the amounts of coronavirus infections worldwide (Amiri, 2021). In Austria the measures proved to be particularly effective among others and one of the most important instruments in Austria was testing (Desson et al., 2020). The World Health Organization recommends all governments to scale up testing for COVID-19. The costs of these tests could be a problem in some countries but a large-scale testing may result in earlier detection of cases, including asymptomatic ones, and thus prevent many new infections and avert hospitalizations (Sousa-Pinto et al., 2020).
Analysis of the financial burden of COVID-19 patient hospitalizations in Austria and Finland over a period of 30 days around the pandemic peak
In the first part of the study the cost of COVID-19 patient hospitalization in the 30-day period of the pandemic first peak per 100,000 population in Austria and Finland were analysed. When calculating the costs, a distinction is made between different categories: ICU beds (Intensive Care Unit) and non-ICU beds. For the current calculation of costs, only prices from the 2020 and 2021 publications were used to reflect the current status in both countries. It should be noted that the calculation of costs for hospitalization is very complex and differs depending on the intensity of the patient’s care. Therefore, the prices used for ICU beds and non-ICU beds should only be regarded as an average value. In addition, the cost categories of the hospital vary nationally and internationally. Data from the University of Washington’s Institute for Health Metrics and Evaluation (IHME) platform were used to analyse and compare health care resources and to calculate the financial burden of hospitalisation for COVID-19 patients. In addition, the first peak of the COVID-19 pandemic in both countries and the associated health care costs were analysed. Both countries were compared in terms of their daily COVID-19 infections and the financial burden of these infections. To obtain further information on the economic outcomes the intensity of social distancing in both countries were analysed. The Data of the University of Washington’s IHME platform was used. In the end of this Article, the results were summarised and discussed with the statements of the researched literature.
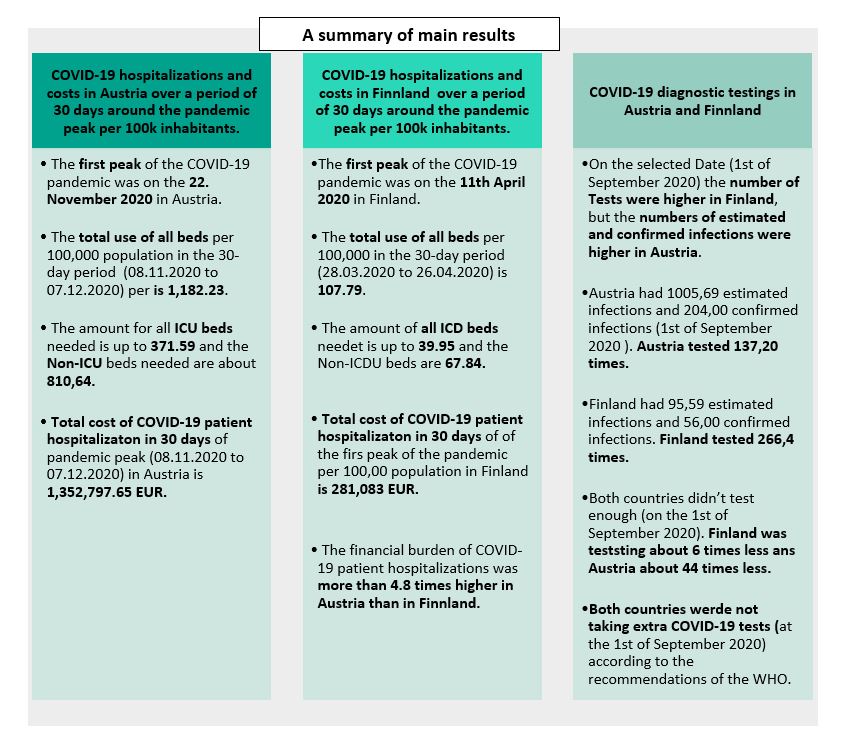
Overview of the main results from the retrospective analysis
The total costs of COVID-19 patient hospitalization in 30 days of pandemic peak (from 08. November 2020 to 07. December 2020) in Austria are 1,352,797.65 EUR. In Finland total costs of COVID-19 patient hospitalization in 30 days of the first peak of the pandemic per 100,00 population (from 28.03.2020 to 26.04.2020) are 281,083 EUR. According to research of this article, a non-ICU hospital bed in Austria costs 923 EUR per day and an ICU bed is about 1,627 EUR. In comparison to that, an ICU bed in Finland costs 3.300 EUR per day and a non-ICU bed costs 2,200 per day. There have been lower hospitalization rates in Finland than in Austria at the height of the corona pandemic. This means the costs in Austria are approximately 4.8 times higher than in Finland in 30 days in pandemic peak. This difference in costs is tremendous, especially due the fact, that costs of hospital resources per day are twice as high in Finland as in Austria.
The comparative analysis between Finland and Austria shows that both countries did not test enough according to the recommendation of the WHO on the 1st of September 2020. For example, on the 1st September 2020 the Austria counts 204 and Finland 56 confirmed infections. The estimated infections were in Austria five times, and in Finland two times higher than the confirmed infections. According to the WHO the optimum test range in Austria was between 2040 and 6120 and in Finland between 560 and 1680 on the 1st September 2020. At this point there were only performed 137.20 tests in Austria and in Finland 266.40 test. However, Finland was testing about 6 times less and Austria in comparison was testing about 44 times less on the 1st of September 2020. The selected countries were not taking extra COVID-19 tests at the 1st of September 2020 according to the recommendations of the WHO.
When analysing the measures of social distancing in both countries, Austria restricts mobility more than Finland. In Austria on the 31st December 2020 the change in mobility is 65% and in Finland 39%. One reason for that result could be that there have been stricter measures in this period in Austria.
Analysing the optimum number of the COVID-19 tests from the economic and clinical perspectives in cross-national level using the IHME, COVID-19 Projection’s data
According to the WHO, the range of optimum COVID-19 tests is around 10 – 30 tests per confirmed case as a general benchmark of adequate testing. Figure 1 shows the number of tests on the 1st of September 2020 in Austria and Finland. The number of tests at this time were higher in Finland, but the numbers of estimated and confirmed infections were higher in Austria (Figure 2 and Figure 3).
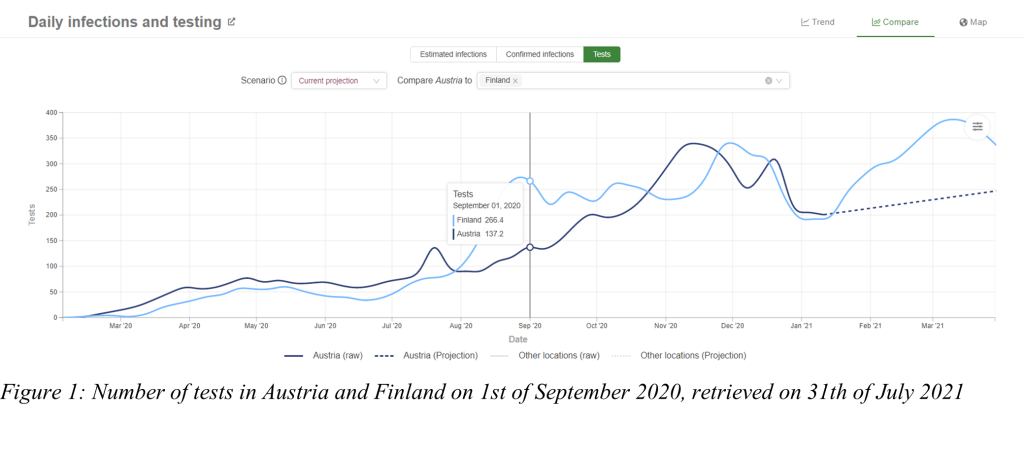
Also, the number of tests is projected after the 13th of January 2021 in Austria, so no more specific numbers can be delivered from this moment on. Figure 2 shows the number of estimated infections on the 1st of September 2020 in Austria and Finland. The number of estimated infections in Austria is several times higher than in Finland. Remember the low gap between the number of tests at the same time in the section above.
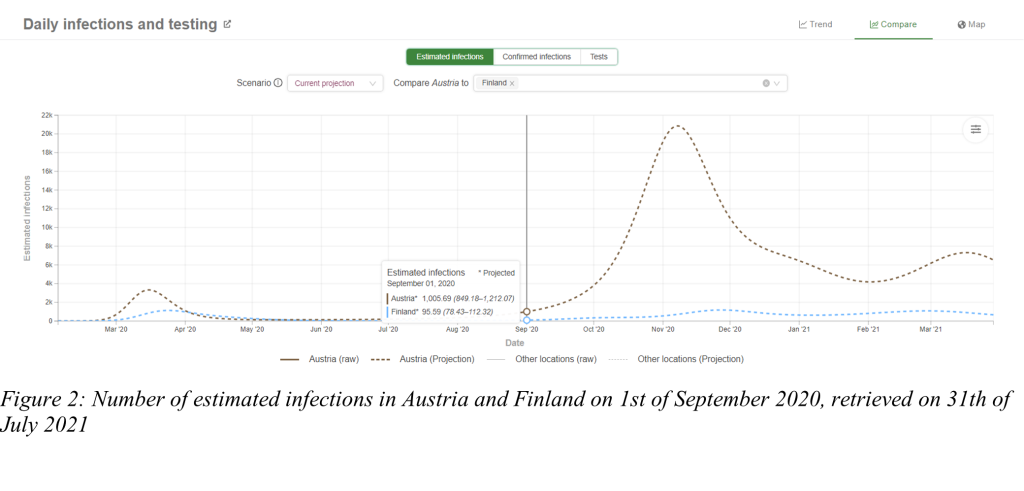
Figure 3 shows the number of confirmed infections on the 1st of September 2020 in Austria and Finland. The number of confirmed infections is also several times higher in Austria than in Finland, like the estimated infections, but the number of tests shows a low gap.
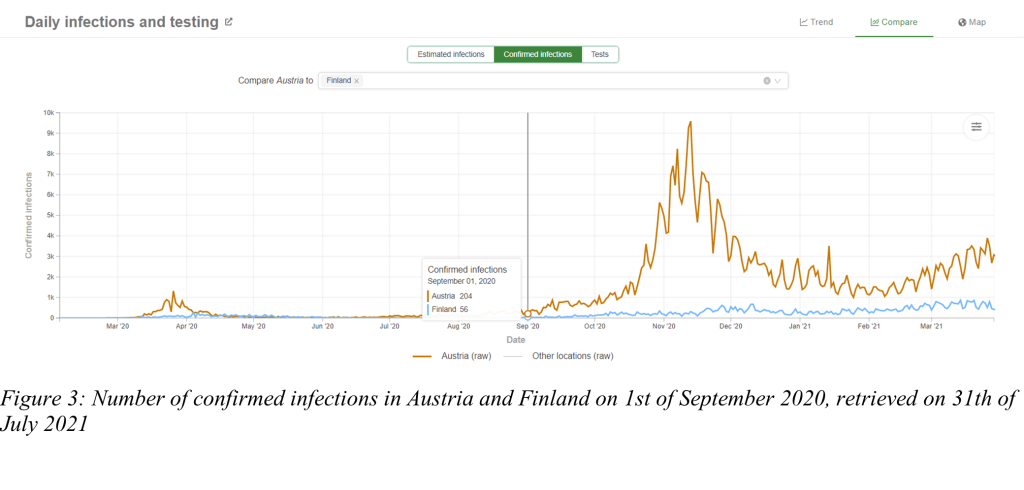
Table 1 shows the comparison of numbers in Austria and Finland, containing tests, estimated infections and confirmed infections on the 1st of September 2020. Also, the recommended tests range for optimum COVID-19 tests is shown in the table.
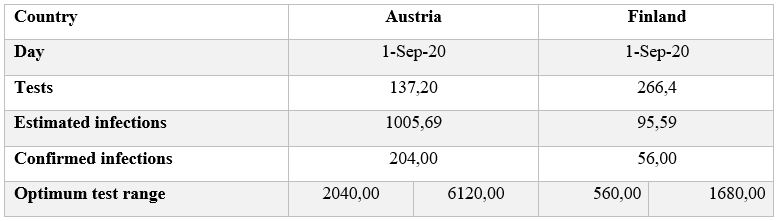
Table 1: comparison of numbers between Austria and Finland
Both countries did not test enough on the 1st of September 2020 according to the recommendation of the WHO. The gap between the number of tests in Austria and Finland on the 1st of September 2020 is low in comparison to the estimated and confirmed infections. According to the recommendation of the WHO for the optimum COVID-19 tests, the number of confirmed infections is multiplied with 10 – 30, meaning a several times higher gap between Austria and Finland in respect to the optimum range of tests. Finland was not testing enough according to the recommendations (about 6 times less), Austria in comparison was testing about 44 times less on the 1st of September 2020.
The selected countries were not taking extra COVID-19 tests at the 1st of September 2020 according to the recommendations of the WHO.
Conclusion
The COVID-19 pandemic does not only affect individual countries such as the countries analysed in the article, Finland or Austria, moreover it affects the whole world. Political, research, health and other leaders are trying to find ways and measures to prevent the spread of COVID-19 and reduce the burden of patient hospitalizations. Policies such as lockdowns, mobility restrictions, social distancing, financial rescue packages, border closures, digital surveillance, political decisions, expert knowledge and research, show that the COVID-19 pandemic is much more than a biological phenomenon. Furthermore, it influences politics, health care, economy, education, geography and society in different forms (Moisio, 2020, 1). The central dimensions of state power in general and the re-production of state power in the practice of health care and economic policy also became visible through the pandemic (Moisio, 2020, 1). Therefore, transparent pandemic risk communication has a great value.
However, the pandemic could be seen as the challenge of the 21st century. According by the WHO by the end of 2020 America was on the highest level with 33 million confirmed infections, more than 23 million cases were confirmed in Europe and more than 11 million cases were confirmed in South-East Asia (Amiri, 2021, 146). Turning to the impact of the pandemic on the health system a huge amount of hospital resources (ICU beds, nursing staff, invasive ventilators worldwide and many more) were needed, to manage these amounts of coronavirus infections (Amiri, 2021, 146). Therefore, analysis of COVID infections and the resulting treatment in hospitals are very essential. In addition, calculating the economic impact of this crisis on individual countries is very important. In this way, long-term political plans can be made for effective measures. These plans and measures must be communicated to society transparently and objectively in a responsible way. As already mentioned, standardised cost accounting methods for the calculation of average hospital unit costs should be critically evaluated, especially with limited data availability and quality. Cost accounting systems already differ among the various health care providers. In addition, cross-country comparisons in terms of ICU bed occupancy and costs are rather rare (Buchegger, 2020, 77). However, the economic assessment of hospitalisation costs plays an important role for healthcare and political decision-makers (Buchegger, 2020, 77).
During the fight against the Virus, the measure of social distancing has become an influential factor. According to the study from Amiri (2021, 146) in Nordic countries social distancing was a successful policy in the containment if the COVID-19 virus. Social distancing leads to lower infection rates, falling mortality and less needed hospital resources for patient hospitalizations (Amiri, 2021, 146). The level of social distancing varied from county to country. However, Finland performs very well in European comparison. The Nordic country continuously implement social distancing policies and a track-and-trace system “with the aim of preventing COVID-19 patient hospitalizations and reducing its burden on healthcare systems” (Amiri, 2021, 146). Austria was also an early adopter of measures such as tracking, testing, social distancing and containment of cases, compared to other European countries (Desson et al., 2020, 406).
In Addition to health system capacity and contact tracing methods a robust testing strategy is also an important tool in containing a pandemic because it builds a foundation for evidence-based decision-making (Desson et al., 2020, 411). The WHO recommends that governments increase the number of tests because studies from different countries showed that large-scale testing was one of the reasons for the flattening of the epidemic curve of new infections and leads to low mortality (Sousa-Pinto et al., 2020, 299). A major barrier to scaling up SARS-CoV-2 testing may be the cost of molecular testing, including the cost of diagnostic kits, analytical equipment and health workers. However, widespread testing strategies lead to earlier detection of cases, including asymptomatic cases. Further is leads to prevention of new infections and a lower amount of hospitalisation (Sousa-Pinto et al., 2020, 299). The costs incurred for testing can be offset in some scenarios by savings in future hospital costs (Sousa-Pinto et al., 2020, 299). Calculating the costs of scaling up testing and hospitalisation of infected persons is very important to ensure sustainable planning of interventions in each country.
References
Amiri, Arshia (2021). Role of social distancing in tackling COVID-19 during the first wave of pandemic in Nordic region: Evidence from daily deaths, infections and needed hospital resources. International Journal of Nursing Sciences 8, 145-151. DOI: 10.1016/j.ijnss.2021.03.010
Buchegger, Stephanie (2020). Analyzing the economic burden of COVID-19 patient hospitalization and testing: A comparison between the Netherlands and Germany. JAMK Journal of Health and Social Studies, 67-78. Access at 18.08.2021 at https://verkkolehdet.jamk.fi/jhss/2020/10/12/buchegger-s-2020-analyzing-the-economic-burden-of-covid-19-patient-hospitalization-and-testing-a-comparison-between-the-netherlands-and-germany/
Desson, Zachary, Lambertz , Lisa, Peters, Jan Willem, Falkenbach, Michelle, Kauer, Lukas (2020). Europe’s Covid-19 outliers: German, Austrian and Swiss policy responses during the early stages of the 2020 pandemic. Health Policy Technol 9(4), 405-418. DOI: 10.1016/j.hlpt.2020.09.003
Moisio, Sami (2020). State power and the COVID-19 pandemic: the case of Finland. Eurasian Geography and Economics, 1-8. DOI: 10.1080/15387216.2020.1782241
Sousa-Pinto, Bernardo, Almeida Fonseca, João, Oliveira, Bruno, Cruz-Correia, Ricardo, Rodrigues, Pedro Pereira, Costa-Pereirab, Altamiro, Rocha-Gonçalvesa, Francisco Nuno (2020). Simulation of the effects of COVID-19 testing rates on hospitalizations. Bull World Health Organ 98, 299. DOI: http://dx.doi.org/10.2471/BLT.20.258186